Supervised by Dr. LaurenScharff
Stephen F. Austin State University
This entire paper contains several sections: Introduction,Changes in Vision and TheirEffects, Impact of LowVision, Available Services,Obstacles to Services, theNeed for Additional Services and anInterdisciplinary Approach, and References.
The visual system changes in many ways as the human body ages.Many visual changes are considered normal while others are consideredpathogenic, or disease-related. While many normal age-related changesoccur in all healthy eyes, many people also suffer fromdisease-related changes that further impair vision. In general, oldereyes are more susceptible to common age-related diseases, such asmacular degeneration, cataracts, and glaucoma. Health problems mayalso make the elderly even more at risk for eye disease, such as thecase of diabetics who develop diabetic retinopathy. Unfortunately,most of the elderly population cannot distinguish between normalvision loss and disease-related vision loss, so many do not seekprofessional care (Silverstone, 1993).
Although both disease-related and normal age-related impairmentsin visual function are important to understand, this project willonly address the issues concerning normal visual changes.
This section will discuss both the anatomical changes andthe neural changes that occur within the visual system withage, as well as the visual effects of these age-relatedchanges.
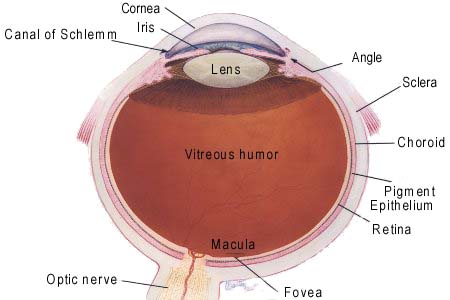
This subsection will discuss the major anatomical changes thataffect the vision of senior citizens. Anatomical changes in the oldervisual system include changes in the lenses, the pupil, the vitreoushumor, the retina, and the retinal pigment epithelium. Thesestructures are labeled in the diagram below.
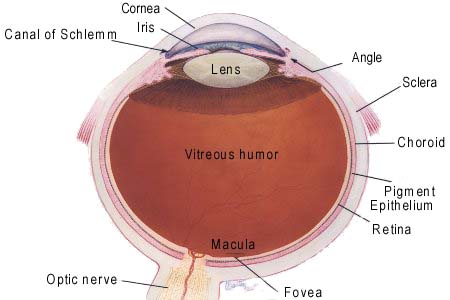
Figure 1: Major structures of the human eye. Although pictured inred, the vitreous humor is a clear fluid. This image is used withpermission from TheColorado Health Site.
The fixed lens, or the cornea, is the first lens thatfocuses the light and, as the most powerful lens in the eye, isresponsible for focusing most of the incoming light. The fixed lensdoes not change shape like the variable lens, but it does go throughchanges with age similar to the variable lens. The cornea thickensover time and adds to the amount of extra light scatter alreadyinside the aging eye (Oberlink, 1997). This thickening can alsoinfluence the focusing power of the fixed lens.
The variable lens (simply called the lens in the diagramabove) is a second lens within the eye and can adjust its shape tofurther focus incoming light. The variable lens begins to change atbirth. As we age, the center of this variable lens loses flexibilityand becomes more rigid (Spector, 1982, p. 34). Over time, thevariable lens loses so much flexibility that it can no longer focuson detailed objects at close range. Although this change occursthroughout the lifespan, adults most often notice it around the ageof forty when the lens can no longer focus on average sized print ata normal reading distance. The chemical composition of the lens alsochanges with time as proteins are produced in different proportions(Spector, 1982, pp. 33-34). These chemical changes cause the lens toyellow over time. This yellowing of the lens reduces itstransparency, causing it to become more opaque with time.
The pupil is the opening in the iris inside the eyethat allows light to enter. As we get older, the pupil gets smallerin diameter (Ordee, Brizzee, & Johnson, 1982, p. 86). This, alongwith the change in variable lens transparency, reduces the amount oflight that the older adult eye receives.
Changes also occur in the vitreous humor, which is thefluid that fills the back of the eye. In young and healthy eyes, thevitreous is a clear gel-like substance with the consistency of eggwhites. With age, the vitreous becomes thinner and more water-like(Balazs & Denlinger, 1982, p. 49). Pockets of liquid vitreousdevelop within the eye (Balazs & Denlinger, 1982, p. 46). Thisliquefied vitreous makes floaters more visible to older individuals.Floaters are clumps of cellular debris that accumulate within the eyeand settle at the bottom of the eye in normal eyes. When the fluidthins, the floaters do not settle and, while seeing the floaters doesnot significantly impair vision, they can be a source of irritationto seniors already dealing with changing vision. Another fairlycommon change that occurs within the vitreous is referred to asposterior vitreous detachment. In older individuals with thiscondition, the thinning vitreous begins to pull away from the retinaat the back of the eye (Balazs & Denlinger, 1982, p. 53). Thisdetachment does not cause any serious impairment alone, but thesymptoms can impact vision. Symptoms include flashes of light,distorted and blurred images, and increased floaters.
The retinal pigment epithelium is a layer of darklypigmented tissue behind the retina. This layer provides the retinawith rich nutrients as well as serving to absorb excess light andprevent light scatter within the eye. In the older human eye, thecells of the pigment epithelium become irregular (Marmor, 1982, p.67). This change means that the pigment epithelium is less able toabsorb excess light and less able to help control light scatter inthe elderly eye. Controlling light scatter in the elderly eye isimportant because light scatter causes glare (Oberlink, 1997).
The term "neural" refers to components of the nervous system,which includes the brain, spinal cord, and nerves. The nervous systemis made up of specialized cells called neurons. Neurons are uniquebecause they are the only cells in the body that communicate throughchemical and electrical signals. Perception relies heavily on thenervous system because neurons pass the information to the brain,which then processes the information.
The retina is an extension of the brain at the back of theeye and is made up of several layers of neurons. The back layer ofthe retina is made up of photoreceptors, special receptor cells thatturn light energy into a neural signal. The loss of retinal cellswith age causes the retina to thin, especially in the periphery. Thecells that survive often exhibit irregular orientations. This changein orientation means that light entering the eye no longer hits thephotoreceptors at the same angle as in younger, healthier eyes(Sekuler, Kline, & Dismukes, 1982, p. 118). This contributes toincreased glare in elderly eyes, which will be discussed further inthe subsection, Visual Effects of Changes.
Other parts of the brain experience cell loss with age as well.Many different neural pathways make up the human brain's visualsystem. Each of these pathways sends sensory information to aspecific part of the brain responsible for a specific aspect ofvision. All of these pathways are likely to lose neurons due to age(Ordy, Brizzee, & Johnson, 1982, p. 86). Because neurons in thebrain do not regenerate, this cell death results in diminishedabilities to perceive different aspects of visual stimuli. Anotherresult of neural cell death is a general slowing of response time,meaning that the visual systems of older persons respond to lightmuch more slowly than younger persons.
Along with changes in the retina, changes in the brain affect theway the aging eye responds to light stimuli. Studies usingelectroencephalograms have provided evidence that reaction times tostimuli increase with age (Ordy, Brizzee, & Johnson, p. 83). Theresults showed that fewer neurons respond to a given stimulus inolder eyes than in younger eyes and that older neurons do not respondas quickly as younger neurons. This change has many effects on theelderly person's ability to perform daily tasks that will bediscussed in further detail in the section Impact of Low Vision onDaily Life.
The brain also undergoes chemical changes that can affect theolder visual system's overall functioning. Neurons throughout thebody communicate through the use of chemicals calledneurotransmitters. When the body produces too many or too fewneurotransmitters, neurons do not communicate properly. As we age,the brain begins to produce neurotransmitters in abnormalproportions. This affects the visual system by changing the abilitiesof neurons in the visual pathways to communicate (Ordy, Brizzee,& Johnson, 1982, p. 85).
The loss of short-term memory is another neural change thataffects vision in older persons (Ordy, Brizzee, & Johnson, 1982,p. 80). This change can impact vision in the elderly when they mustdivide their attention among multiple stimuli. Short-term memory losscan also impair vision when the elderly must organize incomingstimuli. These changes and impairments make several implications forthe senior citizens' ability to drive as well as other tasks. Theseissues will be further discussed in Impact of Low Vision on DailyLife.
While many neural and anatomical changes are independent of eachother, some changes are a combination of both types of change. As aresult of both neural and anatomical changes, the older eye haslimited motility as compared to younger, healthier eyes (Leigh, 1982,pp. 175-176; Lott, et al., 2001). Motility refers to the ability ofthe eye to move properly. Older individuals tend to have less controlover their voluntary eye movements than younger people. Also, theolder eye has a more limited range of movement. Aging eyes have adecreased ability to perform smooth pursuit eye movements, which areused when the eye tries to visually track a moving object. Duringsaccadic eye movements, which are used to scan stationary objects,the eye jumps from one part of the scene to the next. The older eyeperforms the visual jumps used in saccadic eye movements more slowlythan the younger eye. These changes in the ability to control eyemovements can affect a number of tasks, such as reading.
The previous section, Changes in Vision, discussed the anatomicaland neural changes that occur in older persons. While these changesin the visual system are interesting to study and understand, whatmakes the changes most important is their impact on the quality ofthe elderly person's vision. Each anatomical change, neural change,or combination of the two has a corresponding impact on vision.
Older persons experience lower light levels than youngerpersons as a result of decreased illumination within the eye. Thisdecrease is due to a combination of several anatomical changespreviously discussed. The first obstacle light faces is decreasedpupil diameter through which it must enter. The aging variable lensfurther filters light, which is more yellow and opaque than inyounger eyes. Researchers estimate that the elderly retina receivesapproximately one third of the amount of light that a younger retinawould receive (Ordy, Brizzee, & Johnson, 1982, p. 86). This meansthat older persons require much more lighting than younger persons.This need for more light interacts with a greater susceptibility toglare to cause problems in everyday living.
Glare is a common complaint among the low-vision elderly.There are several types of glare, each resulting from an interactionbetween different types of lighting and visual anatomy or anatomicalchanges. Each ultimately causes a different type of visual impairmentas discussed by Carter (1982, p. 122). Veiling glare occurs whenstray light hits the retina uniformly, such as when light from insidea car reflects off the windshield. Scotomatic glare occurs when theeye is overloaded with light and often results in an afterimage, likea camera flash may cause. Dazzling glare can only be noticed insituations with very bright light, such as when looking at thefilament within a light bulb.
The orientation of photoreceptors is an important anatomical issuebecause it influences both the response to incoming light and theperception of glare. In a normal, healthy eye, the photoreceptors areangled so that light entering the eye through the pupil is mostlikely to directly hit the top of the photoreceptors. This phenomenonis referred to as the Stiles-Crawford effect and serves to limit theresponse to light scatter in the healthy eye (Sekuler, Kline, &Dismukes, 1982, p. 118). In older eyes, the photoreceptors havebecome disarranged and abnormally oriented. Photoreceptors that areirregularly oriented are less likely to respond to light thannormally oriented receptors. This is because the light is less likelyto travel through the long axis of the photoreceptor as in normallyoriented cells. When light does not pass through the entire receptor,it is less likely to activate enough of the chemical within the cellto cause it to respond. In older eyes, not only does light enteringthrough the pupil directly hit the top of photoreceptors, but lightbouncing off the aging retinal pigment epithelium and lightscattering as a result of floaters is also likely to directly hit thetop of photoreceptors. Overall, the disorientation of agingphotoreceptors causes the photoreceptors to be less responsive toincoming light but more responsive to scattered light within the eye.The result of this situation is that the older eye will perceive moreglare than the younger eye in the same conditions.
Another visual effect of age-related changes is the inabilityto discriminate colors. The older, yellow lens acts as a filterfor shorter wavelengths (which correspond to purple and blue colors),meaning that these colors will appear dull or even gray. Pastelshades, not matter what color, are difficult to distinguish from oneanother in the elderly eye (Haegerstrom-Portnoy, Schneck, &Brabyn, 1999). Decreased color discrimination results moslty fromcell loss in the fovea (Ordy, Brizzee, & Johnson, 1982, p. 87).The fovea is the small area of the retina where the retinal imagefalls when the eye focuses on something. The fovea is responsible forresolving fine details and it contains densely packed color-sensitivephotoreceptors, called cones. As the eye ages and the foveaexperiences cell loss, important color information is lost. The needfor increased intensity also hampers color discrimination (Carter,1982, p. 122). As the eye ages, it requires greater intensities ofcolor for the visual system to perceive stimuli. Even colors onopposite ends of the color spectrum can be difficult to discriminateif they are of the same intensity.
Poor color discrimination interacts with poor contrastsensitivity to make boundary detection a challenge (Pastalan,1982, p. 324). The term contrast refers to the amount of luminancedifference between to parts of a stimulus, such as text andbackground, or the edges of objects. Contrast sensitivity is ameasurement of the smallest amount of contrast a person can perceive.People with high (good) contrast sensitivity will be able todistinguish two parts of a stimulus with little contrast (i.e. littledifference between the foreground and background), such as dark graytext on a slightly lighter gray background, or light gray text on awhite background. People with low contrast sensitivity, such as theelderly, need high contrast stimuli, such as black text on a whitebackground. Figure 2 below shows examples of high and low-contrastprint. Contrast sensitivity also interacts with size, meaning poorcontrast sensitivity is less of a problem when a stimulus is large.The disabilities resulting from this lowered contrast sensitivitywill be discussed in the next section.
|
High Contrast Text |
| Low Contrast Text |
Figure 2: Examples of high contrast text (top box), where there isa large lightness difference between the text and the background, andof low contrast text (bottom box), where there is little lightnessdifference between the text and the background.
Decreased acuity is probably the most commonly known effectof the older person's anatomical and neurological changes. Acuityrefers to a person's ability to resolve details (i.e. read smallprint) and is the measurement of vision with which most people arefamiliar. Decreased acuity results from a combination of changeswithin the aging eye, including cell loss in the fovea, decreasedtransparency of the vitreous, and increased light scatter and glarewithin the eye (Haegerstrom-Portnoy, Schneck, & Brabyn, 1999).Acuity in the aging eye also depends on the individual's contrastsensitivity. Stimuli with higher contrast will lend itself to higheracuity scores while stimuli with lower contrast will result in loweracuity scores among the elderly.
Return to the front page of thisproject.